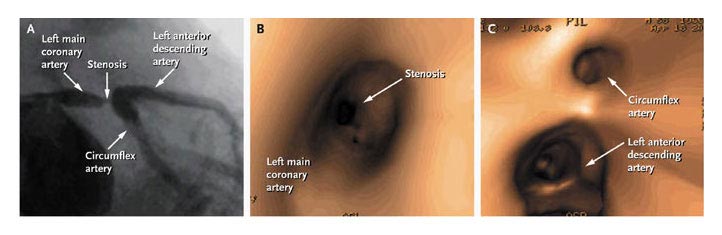
An
angiogram is an invasive test (arteriogram) in which a radiopaque
dye is injected through a catheter inserted into the right femoral
artery located in the groin and carefully placed through the
aorta into the opening of the coronary arteries in order to
visualize the coronary arteries looking for abnormalities such
as narrowing (stricture) due to atherosclerotic plaques and
dilatations (aneurysm) etc.
(see
figures 52, 53, 53a, 54, 55 and 56a).
Complications of Coronary Percutaneous
Angioplasty
Patients undergoing coronary intervention
are subject to the same complications encountered with the performance
of coronary arteriography. In addition, because instrumentation
of the atherosclerotic lesion takes place, coronary artery dissection,
thrombus formation, and coronary artery spasm may occur, leading
to acute occlusion of the coronary artery or of side branches
arising from it. Atheroembolism may occur and lead to MI in
an otherwise successful procedure. Occlusion of the treated
artery is the most common serious complication of coronary angioplasty
and accounts for most of the morbidity and mortality related
to the procedure.
Of Gruentzig’s first 50 patients, 5 experienced an acute
deterioration necessitating emergency bypass surgery and 3 showed
electrocardiographic evidence of MI. The results of 3500 patients
undergoing elective balloon angioplasty at Emory were analyzed
and reported in detail. Angioplasty was attempted in 3933 lesions,
with a success rate of 91 percent. No complications occurred
in 89 percent of patients, minor complications occurred in 6.9
percent, and major complications (emergency surgery, MI, death)
occurred in 4.1 percent. Emergency CABG was performed in 2.7
percent of patients, who had an MI rate of 49 percent and a
0-wave MI rate of 23 percent. In patients sent for emergency
surgery, the mortality rate was 2 percent. The overall MI rate
was 2.6 percent. There were two nonsurgical deaths, giving a
total mortality rate of 0.1 percent (4 of 3500). Five preprocedural
predictors of a major complication were identified: multivessel
coronary artery disease, lesion eccentricity, presence of calcium
in the lesion, female gender, and lesion length.
The strongest predictor of a major complication was the appearance
of an intimal dissection during the procedure. Intimal dissection
was evident in 29 percent of patients, and its presence resulted
in a sixfold increase in the risk of a major complication.
Minor complications tabulated in this study included the following:
side branch occlusion (1.7 percent), ventricular arrhythmia
requiring dc shock (1.5 percent), emergency recatheterization
(0.8 percent), femoral artery repair (0.6 percent), transfusion
requirement (0.3 percent), coronary embolus (0.1 percent), cardiac
tamponade (0.1 percent), and stroke (0.03 percent). This early
series of patients was treated with balloon angioplasty alone.
In 1995 at Emory University Hospital, over 1600 patients were
treated (76 percent with balloon alone), with angiographic success
in 94 percent, Q-wave MI in 1.1 percent, non-Q-wave MI in 2.9
percent, and death in 0.6 percent.
Stents have played an increasing role, being used in 66 percent
of patients in 1998 with an improvement in acute outcome (see
Table 1).
Although angiographic variables are important predictors of
abrupt closure, of equal or greater importance is an estimate
of the consequences of abrupt closure. This estimate is determined
in large part by the amount of myocardium that is supplied by
the artery in jeopardy. Occlusion of a small diagonal branch
is of little consequence compared, for example, with the occlusion
of a large LAD coronary artery that is also supplying collateral
vessels to an occluded right coronary artery. In the first case,
a small non-Q-wave MI is likely, whereas in the latter, occlusion
would likely result in abrupt anterior and inferior ischemia
and be associated with hypotension and possibly cardiogenic
shock.MI will occur in up to one-half of patients, and there
is a significant risk of mortality in this subgroup of patients.
An analysis of 294 acute occlusions occurring
during 8207 consecutive coronary angioplasty procedures performed
in two centers revealed 13 cardiac deaths (4.4 percent of acute
occlusions) and an overall cardiac mortality of 0.16 percent.
Of 13 patients who died, 12 were women. Multivariate analysis
identified three independent predictors of death: collaterals
originating from the dilated vessel, female gender, and multivessel
disease. In an analysis of 32 deaths associated with 8052 PTCA
procedures in three centers, left ventricular failure due to
vessel occlusion, the most common cause of death, was independently
correlated with female sex, “jeopardy score,” and
PTCA of a proximal right coronary artery (RCA) site but not
ejection fraction or presence of multivessel disease. Right
ventricular failure due to occlusion of the proximal RCA and
left main coronary dissections accounted for most of the remaining
deaths.
The use of stents in the course of a failing angioplasty ( Fig.
56j ) and prospectively in patients with unfavorable anatomy
has significantly reduced the risk of urgent bypass surgery
and 0-wave MI. The increasing use of stents and adjunctive measures
including new, powerful antithrombotic agents may herald a “new
era” of coronary intervention. New complications specifically
related to the use of nonballoon devices include coronary perforation,
distal atheroembolization, arterial access complications, and
“domino stenting” (additional stents to treat end-of-stent
dissections). The risk of coronary perforation is a limiting
factor in achieving optimal atherectomy and significantly restricts
use of the TEC device in native vessels. Among 8932 patients
treated at William Beaumont Hospital, perforation was reported
in 0.4 percent (balloon, 0.14 percent; TEC, 1.3 percent; DCA,
0.25 percent; excimer laser 2 percent). This risk of perforation
is highest in tortuous and smaller vessels and in laser angioplasty
of right coronary lesions. In patients experiencing free perforations,
Ellis reported that 75 percent required surgery, 29 percent
had a 0-wave MI, and 14 percent died. Perforation was reported
in 10 of 432 stent patients (2.3 percent), resulting in cardiac
tamponade (50 percent), MI (40 percent), emergency surgery (50
percent), and death (30 percent). The manifestations of perforation
were delayed (5—24 h) in 20 percent of patients. Angiographic
features associated with stent-related perforation were complex
lesion morphology, small vessel diameter (2.6 ± 0.2 mm),
oversized stents (stent/ artery ratio 1.4 ± 0.1), tapering
vessel (40 percent), and recrossing dissections (20 percent).
These results should engender a cautious approach to stenting
in small vessels and when there is uncertainty regarding wire
position. One of the newest causes of perforation is the hydrophilic
coronary guidewire, which easily penetrates the wall of small
distal arteries causing bleeding and cardiac tamponade, especially
when lib/Illa receptor inhibitors have been used. Prompt application
of strategies for the management of vessel perforation can be
lifesaving, and device angioplasty operators must be facile
with them.
Fortunately, the risk of vascular access-site complications,
a frequent accompaniment of stenting when heparin and warfarin
anticoagulation is used adjunctively, has been reduced with
less aggressive antithrombotic strategies. In our experience,
complications at the femoral artery puncture site were more
often related to advanced age, female sex, hypertension, and
postprocedure heparin use than to the size of the catheter.
Prolonged compression of pseudoaneurysms using ultrasound guidance
and in some cases local thrombin injection obviates surgery
in many patients with this complication. Closure devices are
used actively in some centers but add significantly to the cost
of the procedure and have their own complications, including
infection.
Distal coronary atheroembolization is only occasionally recognized
clinically with ballon angioplasty butprobaly occurs moderately
frequently and is a clinically important of debulking srategies
such as atherectomy and laser ablation, where ita, manifestations
are slow coronary flow, ischemia, and infarction. Reports from
CAVEAT indicate that creatine kinase elevations postprocedure
were associated with worse long-term outcomes (death, MI, repeat
intervention). Although procedural modifications with rotational
atherectomy appear to have reduced the immediate impact of microparticulate
embolization, the issue remains a source of concern and needs
further study. Patients at increased risk include those with
bulky or long native vessel lesions and nonfocal or thrombotic
saphenous vein graft lesions, where embolization with TEC was
noted in about 20 percent, and about one-third of patients with
this complication died. Atheroembolization also complicates
stenting, accounting for an increased rate of non-Q-wave MI
compared with balloon angioplasty. Particulate embolism to the
coronary microcirculalion may lead to otherwise silent infarction
reflected by creatine kinase elevation, a topic of intense interest
due to the finding of adverse late outcome, even with small
elevations, and the recognition that lIb/Illa platelet receptor
inhibitors, filters, and occlusion-aspiration” systems
can protect against this complication. Not all studies, however,
have found a correlation between enzyme elevations and adverse
late outcome, and this issue of when to use lIb/Illa platelet
receptors inhibitors is actively debated.
Acute contrast nephropathy requiring dialysis is a costly complication
of coronary intervention, which occurred in 15 of 1828 (0.8
percent) patients and was associated with a high (33.8 percent)
in-hospital mortality. Independent predictors of contrast nephropathy
included decreased baseline creatinine clearance, diabetes,
and contrast dose (no dialysis was required in patients receiving
less than 100 mL of contrast material). Adequate periprocedural
hydration and limitation of contrast volume are the most important
measures in high-risk patients.
TABLE 1. Results of Percutaneous Coronary
Intervention, Emory University Hospital
| |
1980-1987
|
1988-1991
|
1992-1995
|
1996-1998
|
Total
|
|
Patients
|
7254
|
6591
|
6367
|
6417
|
26,629
|
|
Arterial segments treated
|
8885
|
9068
|
8321
|
8342
|
34,616
|
|
Initial success. %a
|
91
|
93
|
94
|
95
|
94
|
|
Complication-free success, %b
|
88
|
90
|
90
|
94
|
91
|
|
Single-vessel disease. %b
|
67
|
49
|
35
|
43
|
48
|
|
Multivessel disease. %c
|
33
|
57
|
65
|
57
|
52
|
|
Multivessel PTCA, %''
|
7.8
|
11
|
9
|
9,5
|
9
|
|
Emergency CABG. %
|
3.4
|
2.1
|
1.3
|
1.5
|
2.1
|
|
Q-wave MI, %
|
1,6
|
1.0
|
0.8
|
0.3
|
1.0
|
|
In-hospital death, %
|
11,2
|
0.5
|
0.6
|
0,7
|
0.5
|
a - Less than 50% residual stenosis.
b - than 50% residual stenosis and freedom from complications.
c - At least 50% stenosis of LAD + RCA. LAD + CIRC, CIRC + RCA,
or LAD + RCA + CIRC.
d - Dilatation of LAD + RCA, LAD + CIRC, CIRC + RCA, or LAD
+ CIRC + RCA.
ABBREVIATIONS: LAD = left anterior descending; RCA right coronary
artery; CIRC = circumflex artery; PTCA = percutaneous transluminal
coronary angiopllasty; CABG= coronary artery bypass graft; MI=
myocardial infarction
Douglas,J.S. and others,PercutaneousCoronary
Intervention,Hurst's The Heart,10th edition Chpt 45 pp.1437-1461.
Samir R. Kapadia, M.D.
Cleveland Clinic Foundation Cleveland, OH 44195
Maria Schlumpf, B.S.
University Hospital Zurich 8006, Switzerland
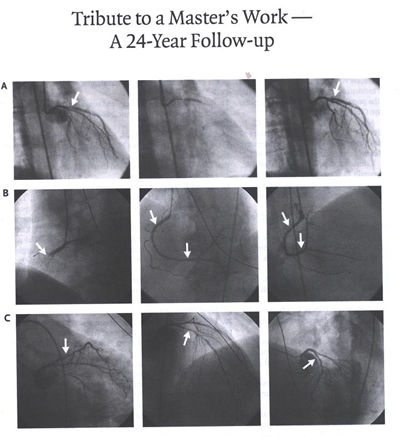
IN APRIL 1978, DR. ANDREAS GRUNTZIG, OF UNIVERSITY HOSPITAL,
ZURICH,
I told a patient who had a tightly narrowed left anterior descending
coronary artery that he did not have enough experience to cite
an accurate success rate for balloon angioplasty of this artery
before he performed the procedure. He said that the patient
was only his eighth, and his first from the United States, to
undergo this procedure. Panel A shows the angiogram from 1978.
The left-hand image shows a lesion in the proximal left anterior
descending coronary artery (arrow), the middle image shows the
balloon inflation, and the right-hand image shows the result
after the balloon angioplasty, with minimal residual stenosis
(arrow). For the next 24 years, the patient enjoyed excellent
health and remained physically very active. In April 2002, he
presented with an acute myocardial infarction of the inferior
wall. Angiography showed total occlusion of the right coronary
artery (Panel B, left-hand image, arrow); two severe lesions,
including the total occlusion, were successfully stented (Panel
B, middle and right-hand images, arrows). Amazingly, the left
anterior descending coronary artery was patent, with no recurrence
of disease (Panel C, arrows). The patient is now 76 years old.
Copyright © 2004 Massachusetts Medical Society
N ENGL J MED 351;13 SEPT23,2004