The
evaluation of the venous pulse is an integral part of the physical
examination since it it reflects both the mean right atrial
pressure and the hemodynamic events in the right atrium. Factors
influencing the right atrial and central venous pressure (CVP)
includes to total blood volume, the distribution of blood volume,
and right atrial contraction . Venous blood returning from the
systemic capillaries is nonpulsatile.Changes in flow and pressure
caused by skeletal muscles and respiratory pump are nonsynchronous
with the pulsatile activity of the heart. Changes in flow and
pressure caused by right atrial and ventricular fillingl, however,
produce pulsations in the central veins that are transmitted
toward the peripheral veins, opposite to the direction of blood
flow. With the possible exception of the "c" wave, which is
the combined result of carotid arterial impact and upward movement
of the tricuspid valve, the pulsations observed in the neck
are produced by right atria and ventricular activity.
Examination of the Jugular Venous Pulse
The two main objectives of the bedside examination
of the neck veins are the estimation of the CVP and the inspection
of the waveform. Usually the right internal jugular vein is
superior for both purposes. In most normal subjects , the maximum
pulsation of the internal jugular vein is observed when the
trunk is inclined by less than 30°. In patients with elevated
venous pressure, it may be necessary to elevate the trunk further,
sometimes as much as 90°. W hen the neck muscles are relaxed,
shining a beam of light tangently across the skin overlying
the internal jugular vein exposes its pulsations Simultaneous
palpation of the left carotid artery aids the examiner in deciding
which pulsations are venous.
Measurement of Venous Pressure
The difference between venous distention and
venous pressure elevation must be considered. Veins may be markedly
dilated with minimal increase in pressure or may not be visible
distended despite a very high venous pressure. Venous pressure
maybe estimated by examining the veins in the dorsum of the
hand. With a patient lying or sitting in a 30° elevation or
greater, the arm is slowly and passively raised from a dependent
position. When the venous pressure is normal, the veins collapse
when the dorsum of the hand reaches the level of the angle of
Louis. Unfortunately, a local venous obstruction or augmented
peripheral venous constriction may diminish the accuracy of
estimating CVP by this method.
The external or internal jugular vein may
also be used to estimate venous pressure. Because of its more
direct route to the right atrium, the internal jugular vein
is superior for the estimation of venous pressure and assessment
of venous waveform. The patient is examined at the optimum degree
of trunk elevation for visualization of venous pulsations. The
vertical distance from the top of the oscillating venous column,
to the level of the sternal angle is generally less than 3 cm.(3cm+5
cm)=8cm). Greatly elevated venous pressure may be missed by
failing to elevate adequately the patient's head. It may be
necessary to actually have the patient sit upright. If the "pulsating
meniscus" is very high, pulsations may be inappropriate in the
lower neck .When venous engorgement is marked the patient's
earlobe may pulsate and even the veins on the top of the head
maybe be distended. In patients suspected of right ventricular
failure but having normal resting venous pressure, the abdominojugular(
also known as the hepatojugular) test is useful. With the patient
breathing normally, firm pressure is applied with the palm of
the hand to the right upper quadrant of the abdomen for 10 or
more s.The patient should be instructed to continue breathing
normally during the test. In most subjects the venous pressure
is not altered significantly. In some normal patients there
is a transient increase in jugular venous pressure with the
"rapid return" to or near baseline in less than 10 s. The dysfunctioning
right ventricle, however, is unable to accept the increment
of blood volume due to enhanced venous without of marked increase
in its filling pressure, which is transmitted to the neck veins.
In patients with right ventricular failure, which often results
from left- sided heart failure, the venous pressure either rises
rapidly and declined slowly during abdominal compression or
remains elevated by 4 or more centimeters of blood until pressures
released (figure 203-a). Ducas et al. studied the abdominal
jugular test and attested to the accuracy of the test results.
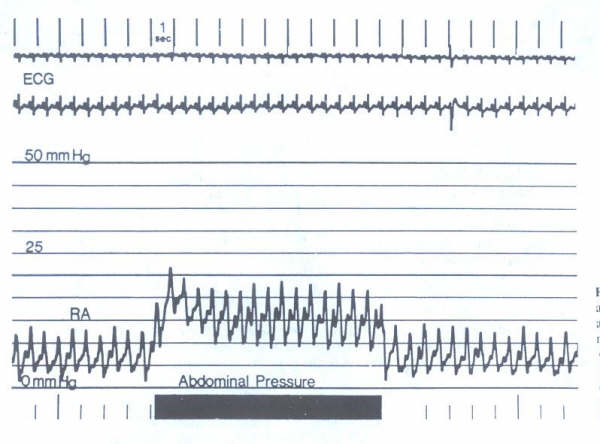
Figure 203-a: Elevation
in right atrial (RA) pressure observed during abdominal pressure
in patient with mild congestive heart failure. (From GA Ewy:
The abdominojugular test:Technique and hemodynamics correlates.
Ann Intern Med 109:456,1989.
Analysis of Venous Waveforms
Again the patient's trunk should be inclined
to whatever elevation is necessary to reveal the top of the
oscillating venous column. Having the patient take a slow deep
inspiration will increase the amplitude of the presystolic 'a'
wave while decreasing the mean right atrial pressure. This is
a useful technique for identifying the site at which the pulsations
will be best visualized. Simultaneous palpation of the left
carotid artery aids the examiner in relating the venous pulsations
to the timing of the cardiac cycle.
Normal Venous Pulse
The normal venous pulse (JVP) reflects phasic
pressure changes in the right atrium and consists of three positive
waves and to negative troughs ( figure 203-b).In considering
this pulse it is useful to refer to the events of the cardiac
cycle. The positive presystolic "a" wave is produced by right
atrial contraction and is the dominant wave in the JVP particularly
during inspiration. During atrial relaxation, the venous pulse
descends from the summit of the "a" way Depending on the PR
interval, this descent may continue until a plateau ("z" point)
is reached just prior to right ventricular systole. More often
the descent is interrupted by a second positive venous wave,
"c" wave, which is produced by a bulging of the tricuspid valve
into the right atrium during right ventricular isovolumic systole
and by the impact of the crowded artery adjacent to the jugular
vein. Following the summit of the "c" wave, the JV P contour
declines, forming the normal negative systolic wave, the "x"
wave. The "x" descent is due to a combination of atrial relaxation,
the downward displacement of the tricuspid valve during right
ventricular systole, and the ejection of blood from both the
ventricles.
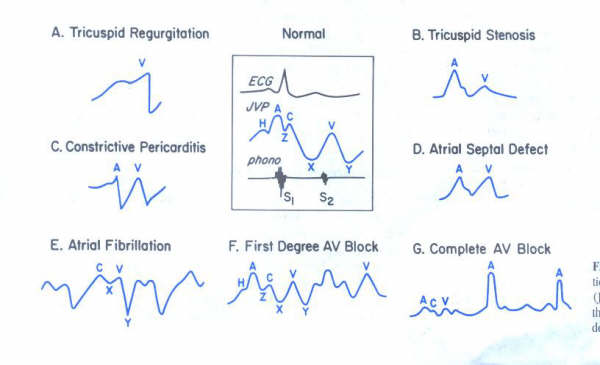
Figure 203-b: Schematic
representation of the normal jugular venous pulse (JVP), four
types of abnormal JVPs, and the JVPs in three arrhythmias. See
text for definition of H,Z,C,X, V, and Y.
The positive, late systolic "v" wave in the
JVP results from the increase in blood volume in the venae cavae
and the right atrium during ventricular systole when the tricuspid
valve is closed. After the peak of the "v" wave is reached,
the right atrial pressure decreases because of the diminished
bulging of the tricuspid valve into the right atrium and the
decline in right ventricular pressure which follow tricuspid
valve opening The latter occurs at the peak of the "v" wave
in the JVP. Following the summit of the "v" wave, there is a
negative descending limb, referred to as the "y" descent or
diastolic collapse, which is due to the tricuspid valve of opening
in the rapid and flow of blood into the right ventricle. The
initial "y" descent corresponds to the right ventricular rapid
filling phase. The trough of the "y" wave occurs in early diastole
and is followed by the ascending limb of the "y"wave, which
is produced by continued diastolic inflow of blood into the
right side of the heart. The velocity of this ascending pressure
curve depends on the rate of venous return and the distensibility
of the chambers of the right side of the heart. When diastole
is long, the descending limb of the "y" wave is often followed
by a small, brief, positive wave, the "h" wave, which occurs
just prior to the next "a" wave. At times, there is a plateau
phase rather than a distinct "h" wave. With increasing pulse
rate the "y" trough and the "y" ascent are followed immediately
by the next "a "wave.( see plate 204. ) Usually, there three
visible major positive waves ("a", "c", "v") and two negative
wave ("x", "y") when the pulse rate is below 90 beats per minute
and the PR interval is normal. With faster heart rates there
is often fusion of the some of the pulse waves and an accurate
analysis of the waveform is more difficult.
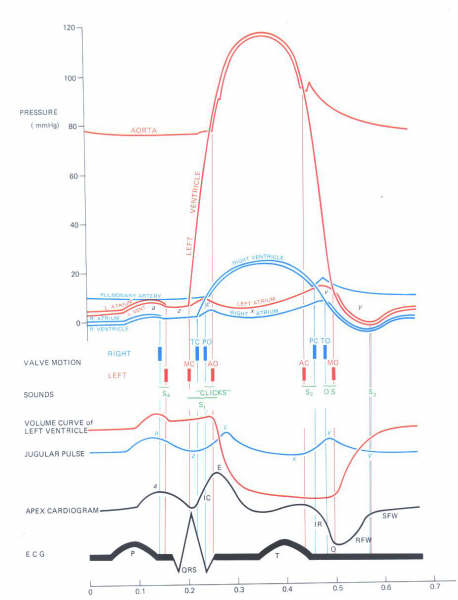
Plate 204:
Diagram of the cardiac cycle,
showing the pressure curves of the great vessels and cardiac
chambers, valvular events and heart sounds, left ventricular
volume curve, jugular pulse wave, apex cardiogram, and the electrocardiogram.
For ilustrative purposes, the time intervals between the valvular
events have been modified and the "Z" point has been
prolonged. Valve motion: MC= mitral component of the first sound;
MO= mitral valve opening: TC=tricuspid component of the first
heart sound;TO=tricuspid valve opening: AC=aortic component
of the second heart sound:AO=aortic valve opening; PC= pulmonic
valve component of the second heart sound; PO= pulmonic valve;
OS= opening snap of atrioventricular valves. Apex cardiogram:IC=isovolumic
or isovolumetric relaxation wave; O= opening of mitral valve;
RFW = rapid- filling wave; SFW=slow filling wave.
Abnormal Venous Pulse
Elevated Venous Pressure
The most common cause of elevated jugular
venous as pressure is an increase right ventricular pressure
such as occurs in patients with pulmonary stenosis , pulmonary
hypertension, or right ventricular failure secondary to right
ventricular infarction. The venous pressure also is elevated
when obstruction to right ventricular inflow occurs,such as
with tricuspid stenosis or right atrial myxoma, or when constructive
pericardial disease impedes right ventricular inflow. It may
also result from vena caval obstruction and, at times an increase
blood volume. Patients with obstructive pulmonary disease may
have an elevated venous pressure only during expiration.
Kussmal's Sign
Normally there is an increase in the "a" wave
of the JVP but a decrease in the mean jugular venous pressure
during inspiration as result of the increase filling of the
right side chambers associated with the decline in intrathoracic
pressure.An inspiratory increase in venous pressure may occur
in patients with severe constrictive pericarditis when the heart
is unable to accept the increase in right ventricular volume
without a marked increase in the filling pressure. Although
Kussmaul's sign was first described in patients with constructive
pericarditis , its most common cause is severe right-sided heart
failure, regardless of etiology. The presence of Kussmaul's
sign is also useful in the diagnosis of right ventricular infarction.
Abnormalities of the "a" Wave
The "a" wave in theJVP is absent when there
is no effective atrial contraction, such as in atrial fibrillation(
figure 203-e ). In certain other conditions, the "a" wave may
not be apparent. In sinus tachycardia the "a" wave may fuse
with the preceding "v" wave, particularly if the PR interval
is prolonged. In some patients with sinus tachycardia, the "a"wave
may occur during the "v" or "y" descent and may be small or
absent. In the presence of first-degree AV block, a discreet
"a" wave with ascending and descending limbs is often completed
prior to the first heart sound and the ac interval is prolonged(
figure 203-f).
Large "a" waves are of considerable diagnostic
value (figure 203-b ). When giant "a" waves are present with
each beat,the right atrium is contracting against an increased
resistance. This may result from obstruction at the tricuspid
valve( tricuspid stenosis or atresia,right atrial myxoma or
conditions associated with increased resistance to right ventricular
filling. A giant "a" wave is more likely to occur in patients
with pulmonary stenosis or pulmonary hypertension in whom both
the atrial and right ventricular septa are intact. Cannon "a"
waves occur when the right atrium contracts while the tricuspid
valve is closed during right ventricular systole. Cannon waves
may occur either regularly or irregularly and are most common
in the presence of arrhythmias (figure 203-g ).
Abnormalities of the "x" Wave
The most important alteration of the normally
negative systolic collapse("x" wave) of the JCP is its obliteration
or even replacement by a positive wave. This is usually due
to tricuspid regurgitation. Although atrial relaxation may contribute
to the normal "x"descent ,the development of atrial fibrillation
does not obliterate the "x" wave except in the presence of tricuspid
regurgitation. Accordingly, the occurrence of a positive wave
the JVP during ventricular systole is strong evidence of tricuspid
regurgitation (figures 203-a and 204). mild tricuspid regurgitation
lessens and shortens the downward "x" wave as the regurgitation
of blood into the right atrium produces a positive wave that
diminishes the usual systolic fall in venous pressure. In some
patients with moderate tricuspid regurgitation, there is a fairly
distinct positive wave during the ventricular systole between
the "c" and "v" waves. This abnormal systolic waveform is usually
referred to as a "v" or "cv" wave, although it has also been
referred to as "r "(regurgitant) or an "s"(systolic) wave. In
patients with constricted pericarditis the "x" descent wave
during systole is often more prominent than the early diastolic
"y" a wave (figure203-c ).
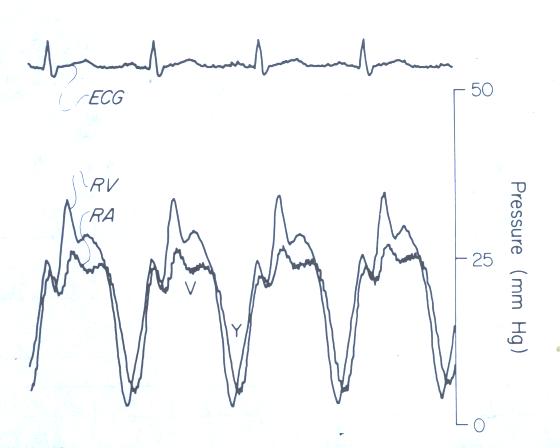
Figure 204:
Right ventricular (RV) and right
atrial (RA) pressure curves and simultaneous ECG form a patient
with severe tricuspid regurgitation. Note vdntricularization
of the RA pressure curve.
Abnormalities of the "v" Wave
The positive, late systolic "v" wave results
from the increasing right atrial blood volume during ventricular
systole when the tricuspid valve normally is closed. With mild
tricuspid regurgitation, the "v" wave becomes more prominent,
and when tricuspid regurgitation becomes severe, the prominent
"v" wave and the obliteration of the "x" descent results in
a single, large positive systolic wave (ventricularization)
( figures203-a and 204 ). Normally the "v" wave is lower in
amplitude than the "a" wave in the JVP. In patients with an
atrial septal defect, however, the higher left atrial pressure
is transmitted to the right atrium and the "a" and "v" waves
are often equal in the right atrium and the JVP (figure 203-d).
In patients with constrictive pericarditis and sinus rhythm
the right atrial "a" and "v" waves may also be equal, but the
venous pressure is increased, which is unusual with isolated
atrial septal defect. In patients with constrictive pericarditis
who are in atrila fibrillation, the "cv" wave is prominent and
the "y"descent rapid .
Abormalities of the "y" Trough
The "y" descent , or diastolic collapse, is
usually is produced mainly by the tricuspid valve opening and
the rapid inflow of blood into the right ventricle. A rapid
deep "y" descent in in early diastole occurs with severe tricuspid
regurgitation (figure 203-a blank).A venous pulse characterized
by a sharp "y" trough, and a rapid ascent to the baseline is
seen in patients with constrictive pericarditis or with severe
right -sided heart failure. A slow "y" descent in the JVP suggests
an obstruction to right ventricular filling and may be the only
abnormal finding in patients with tricuspid stenosis or right
atrial myxoma (figure203-b). In both constrictive pericarditis
and severe right-sided heart failure, the venous pressure is
elevated with a sharp "y "dip in the JPD. The presence of a
large positive systolic venous wave favors the diagnosis of
severe heart failure.
Effects of Arrhythmias of the Venous Pulse
The large "a" waves in the JVP during arrhythmias
are present when the P wave (atrial contraction) occurs between
the onset of the QRS complex and determination of the T wave
(figure 203-g ). Such cannon "a" waves may occur regularly in
junctional rhythm. More commonly, they occur irregularly when
AV dissociation accompanies premature ventricular contractions,
ventricular tachycardia, or complete heart block. The "a" wave
is absent in patients with atrial fibrillation, and flutter
"a" waves at a regular rate of 250 to 300 per minute frequently
are observed in patients with atrial flutter and varying degrees
of AV block. Patients with multifocal atrial tachycardia often
have prominent and somewhat variable "a" waves in the JCP. In
these patients, many of whom have pulmonary hypertension secondary
to lung disease, the "a" waves are often very large.
Reference:O'Rourke,R.A.and Others,General Examination
of the Patient,Hurst's, The Heart,Eighth Edition,Pp.238-242.