There are three types of apnea: obstructive,
central, and mixed; of the
three, obstructive is the most common. Despite the difference
in the
root cause of each type, in all three, people with untreated
sleep apnea
stop breathing repeatedly during their sleep, sometimes hundreds
of
times during the night and often for a minute or longer.
Obstructive sleep apnea (OSA) is caused by
a blockage of the airway,
usually when the soft tissue in the rear of the throat collapses
and
closes during sleep.
In central sleep apnea, the airway is not
blocked but the brain fails to
signal the muscles to breathe.
Mixed apnea, as the name implies, is a combination
of the two. With each
apnea event, the brain briefly arouses people with sleep apnea
in order
for them to resume breathing, but consequently sleep is extremely
fragmented and of poor quality.
OBSTRUCTIVE SLEEP
APNEA
Approximately 30 million Americans are
victims of a sleep disorder
called obstructive sleep apnea. Many millions more are predisposed
and
have a high risk of developing the illness. If you are an adult
male,
the odds are about 50/50 that your breathing is not normal when
you are
sleeping. It is imperative that anyone who might have this problem
or is
predisposed, or knows someone they care about who has the problem,
should have the clearest possible understanding about it.
DETAILED DESCRIPTION OF ALL ASPECTS
Of OBSTRUCTIVE SLEEP APNEA
1. What is Obstructive Sleep Apnea (OSA)?
People with OSA experience recurrent episodes
during sleep when their
throat closes and they cannot suck air into their lungs (apnea).
This
happens because the muscles that normally hold the throat open
during
wakefulness relax during sleep and allow it to narrow(osa-fig5).
When
the throat is partially closed and/or the muscles relax too
much, trying to inhale will suck the throat completely closed
and air cannot pass at
all (osa-figures5,6,6b,6c). This is an obstructive sleep apnea
episode
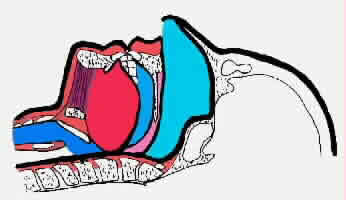
Figure5: Obstructive sleep apnea (OSA) is caused
by the closing of the upper airway while asleep.
The uvula and
soft pallet collapses on the back wall of the upper airway.
Then the tongue falls backward, collapsing on the back wall
of the upper airway, the uvula and soft pallet forming a tight
blockage, preventing any air from entering the lungs. The effort
of the diaphragm, the chest and the abdomen only cause the blockage
to seal tighter. In order to breathe the person must arouse
or awaken, causing tension in the tongue thereby opening the
airway, allowing air to pass into the lungs.
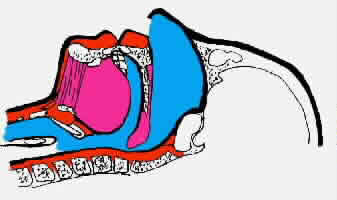
Figure 6: Snoring showing a partially closed
upper airway
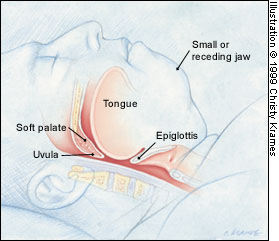
osa-fig 6c: Abnormal airway during sleep.
Multiple
sites of obstruction often occur in patients with obstructive
sleep apnea. An elongated and enlarged soft palate impinges
on the posterior airway at the level of the nasopharynx and
oral pharynx. In addition, a retruding jaw pushes an enlarged
tongue posteriorly to impinge on the hypopharyngeal space.
A cessation of breathing must last 10 seconds
or more to be called an
apnea. Obstructive apnea episodes can last as long as two minutes
and
are almost always associated with a reduction in the level of
oxygen in
the blood. When an individual is in the midst of an obstructive
sleep
apnea episode, as long as sleep continues, the apnea continues.
It is
only terminated and the victim's life is saved by waking up.
This
arousal instantly increases the activity of the muscles of the
tongue
and throat muscles that enlarge the airway. The victim will
be able to
breathe and to once again fill the lungs with life-giving oxygen.
This
cycle may be repeated hundreds of times a night while the sufferer
has
no idea it is happening.
2. What are the cardinal symptoms?
a) Fatigue and tiredness during the day.
b) Loud snoring; if the loud snoring is repeatedly punctuated
by brief
periods of silence or choking sounds, the individual is certain
to have
obstructive sleep apnea.
3. Other common features are:
a) Obesity
b) Small jaw, thick neck


osa-fig 6f. A 24-year-old woman with facial
abnormalities that contribute toobstructive sleep apnea.
(Lower) The receding
lower jaw provides inadequate support for the lower lip, resulting
in lip curling and a deep mental-labial fold (curved arrow).
(Upper) Shortness of the lower one third of the face
(arrows) contributes to inadequacy of the airway.
c) High blood pressure
OSA is now recognized to be an independent risk factor for daytime
hypertension (osa-fig4).
osa-Figure 4 Dose-response relationship between the severity
of
obstructive sleep apnea based on apnea-hypopnea index and the
adjusted
odds ratio of hypertension, defined as blood pressure >140/90
mm Hg or
current treatment with antihypertensive medications. Odds ratio
was
adjusted for baseline hypertension status, age, gender, habitus,
and
weekly alcohol and cigarette use. P= 0.002 for linear trend
of the
logistic regression coefficients. data from Peppard et al.
d) Restless sleep; the repeated struggle to breath can be associated
with a great deal of movement.
e) Depressed mood and/or irritability
f) Reduced sex drive and impotence
g) Snorting, gasping, choking during sleep
4. Not as commonly reported but may
be present:
Feeling that sleep is strangely unrefreshing
Difficulty concentrating
A dry mouth upon awakening
Excessive perspiration during sleep
Heartburn(gastroesophageal reflux)
Rapid weight gain
Morning headaches
Change in personality
Memory lapses
Intellectual deterioration
Frequent nocturnal urination (nocturia)
Confusion and severe grogginess upon awakening
Specially in young children, large tonsils and adenoids.
There may be chest retraction during sleep (the sternum and
the
spaces between ribs pull unnaturally inward when trying to inhale)
4. How serious is OSA?
Depending on the degree of severity, OSA is
a potentially
life-threatening condition. Someone who has undiagnosed severe
obstructive sleep apnea is likely to have a heart attack, a
stroke,
cardiac arrest during sleep, or a harmful accident(osa-fig.3)
Figure 3. Prevalence of obstructive sleep apnea (OSA) in patients
with
cardiovascular and cerebrovascular disease.
The figures used
are
approximations from published data and are unadjusted for baseline
variables (1 to 4):
1. Parati G, Ongaro G, Bonsignore SIR, Glavina
F, Di
Rienzo M, Mancia G. Sleep apnoea and hypertension. Curr Opin
Nephrol
Hypertens 2002; 11:201-14;
2. Sin DD, Fitzgerald F, Parker JD,
Newton G,
Floras JS, Bradley TD. Risk factors for central and obstructive
sleep
apnea in 450 men and women with congestive heart failure. Am
J Respir
Crit Care Med.1999;160:1101-6;
3.Bassetti C., Alrich, Ms .Sleep
apnea i
acute cerebrovascular diseases:final report on 128 patients. Sleep
999;22:217-23;and
4.Peker Y. and others. An independent assoiation
between obstructive sleep apnea and coronary artery disease.Eur.Respir.J
1999;14:179-84.
Sleep apnea has clearly been demonstrated to be an independent
risk
factor for hypertension.More importantly,all published studies
have
shown that a large proportion(40% to 80%) of stroke patients
have
OSA, suggesting it may increase the stroke risk beyond direct
effects on
blood pressure level and variability.
Patients with OSA have many features in common
with the metabolic
syndrome, including systemic hypertension(osa fig.2), central
obesity,and
insulin resistance(due to increased sympathetic nerve activity).
Figure 2 Sympathetic nerve activity increases through the
obstructive
apnea, resulting in marked vasoconstriction followed by increased
systolic and diastolic blood pressure.
Continuous positive airway
pressure (CPAP) stabilizes both sympathetic activity and blood
pressure
surges. BP = blood pressure (mm Hg); OSA = obstructive sleep
apnea; REM = rapid eve movement; RESP = respiration; SNA = sympathetic
nerve
activation. permission.
The risk of experiencing angina or an acute
coronary syndrome is
increased in the hours after waking from sleep.
Strong evidence of a link between snoring
and stroke now exist from
case-controlled studies.
Arrhythmias and risk of causes of cardiovascular
morbidity in OSA
patients appears related to the severity of sleep apnea.
Obstructive apnea is common in heart failure
patients.40% of these
patients had CSA (central sleep apnea),which differs from OSA
in that
there is periodic cessation of breathing with no "respiratory
effort",followed by hyperventilation.The key mechanisms
of periodic
breathing in heart failure patients are enhanced chemoreflex
sensitivity,hypocapnia ,and unstable breathing control,especially
during sleep.
Patients with heart failure can have a combination of CSA and
OSA.
Acute pulmonary hypertension changes during
obstructive apneas are well
defined but the extent to which these tranlate into permanent
daytime
PHT remains less certain.
In addition, awakening to breathe hundreds
of times in a single night
causes the victim to become very sleep deprived. There is a
constant
risk of serious accidents such as falling asleep while driving
as well
as impaired function in the workplace and in personal relationships.
All
of the negative consequences of OSA increase as severity increases.
Untreated OSA tends to progressively worsen
and sooner or later will
result in partial or complete disability and death.
5. Risk Factors
a) The primary risk factor for OSA is excessive
weight gain(see osa-fig 6b below). The accumulation of fat on
the sides of the upper airway causes it to become narrow and
predisposed to closure when the muscles relax.

osa-fig 6b An obese young woman with the short,
thick neck typically seen in patients with obstructive sleep
apnea.
b) Age is another prominent risk factor. Loss
of muscle mass is a
common consequence of the aging process. If muscle mass decreases
in the
airway, it may be replaced with fat, leaving the airway narrow
and soft.
c) Men have a greater risk for OSA. Male
hormones can cause structural
changes in the upper airway.
d) Other predisposing factors associated
with OSA include:
e) Anatomic abnormalities, such as a receding
chin

osa-Fig.6h.A 36-year-old woman with facial
abnormalities that contribute to obstructive sleep apnea. Note
the small, receding jaw (black arrows), as well as the moderate
curling of the lower lip and the deep mental labial fold (white
arrow).
f) Enlarged tonsils and adenoids, the main
causes of OSA in children
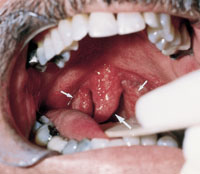
osa-fig 6d Enlarged uvula resting on the base
of the tongue (large arrow), along with hypertrophied tonsils
(small arrows). The posterior pharyngeal erythema may be secondary
to repeated trauma from snoring or gastroesophageal reflux

osa-fig 6e Elongated soft palate (arrows).
In this patient, an increased anteroposterior dimension caused
the soft palate to rest on the base of the tongue in the relaxed
position.
g) Family history of OSA, although no genetic
inheritance pattern has
been proven
h) Use of alcohol and sedative drugs, which
relax the musculature in
the surrounding upper airway
i) Smoking, which can cause inflammation, swelling, and narrowing
of
the upper airway
j) Hypothyroidism, acromegaly, amyloidosis,
vocal cord paralysis,
post-polio syndrome, neuromuscular disorders, Marfan's syndrome,
and
Down syndrome
k) Nasal congestion
DIAGNOSIS OF
OSA
If you suspect that you may have OSA, what
should you do?
1) You must first become as knowledgeable
as possible about OSA yourself.
2) You can also do a number of simple things that will convert
your
suspicions into certainty.
3) The best first step is to involve your
spouse or other family member. He
or she can audiotape or videotape you while you are sleeping.
The sounds
and repeated silences and struggles to breath are highly characteristic.
4) When you have enough ammunition, make an
appointment with your
physician specifically to get help for your OSA. Your spouse
must
accompany you if at all possible.
5) Polysomnography is the "gold standard"
diagnostic tool for assessing
sleep-disordered breathing.
It requires an overnight stay at a sleep laboratory,
with monitoring of
oxygen saturation, heart rate, sleep stage by electroencephalography,
nasal airflow, oral airflow, jaw muscle tone by electromyography,
sleep
position, and chest and abdominal
movement.
Measurement of these parameters allows diagnosis
of the type
of sleep-disordered breathing and its severity. The apnea-hvpopnic
index
(AHI)-the number of obstructive events per hour-is the most
commonly
used measurement to quantify OSA:mild OSA = 5-15 events/h;moderate=15
to 30 events/h; and severe > 30 events/h.A "negative"
polysomnographic
study does not exclude mild OSA,however,because there is night-to-night
variability in the frequency of obstructive events(osapolysomnography-Fig.1).

oaspolysomnograghy-figure 1 Polysomnography: an overnight
summary.
The graphs from the top are:
1) hypnogram: the sleep
stage report (MOV AWK = movement when awake; REM = rapid eye
movement; 1 to 4 = non-rapid eye movement sleep);
2) arousals:
each is a single mark;
3) SaO2 =
percentage oxygen saturation;
4) apnea score: each is a single
mark
(Cn.A = central apnea; Ob.A -_- obstructive apnea; M4x.A = mixed
apnea;
Hyp = hypopnea; Uns =unscored);
5) PLMS=paroxysmal limb movements;
6)
heart rate versus time(beats/min.);
7) body position: this subject
remained on
his back throughout the study; and
8) time(h).
All patients with hypertension,obesity, or heart failure should
be asked
routinely asked about OSA(see paragraphs 2-4 above describing
cardinal
symptoms and referred for a sleep study if they are symptomatic.
The Epworth Sleep Scale standardizes these questions and these
by
providing a rapid,validated method of screening for tiredness
and is
useful in both clinical practice and research settings.
Table 1. Epworth Sleepiness Scale
Situation
Sitting and reading
Watching TV
Sitting in an inactive place (e.g., movie)
As a passenger in a car without a break for an hour
Lying down to rest in the afternoon when the circumstances permit
Sitting and talking to someone
Sitting quietly after lunch without alcohol
In a car, while stopped for a few minutes
Scale--------------------------------------------------- Score
No chance of dozing-----------------------------------0
Slight------------------------------------------------------
1
Moderate------------------------------------------------- 2
High--------------------------------------------------------
3
(Score for each situation is added to total)
Total
<-6 = Less tired than average
7-8 = Average
<-9 = Tiredness requiring investigation
How is sleep apnea treated?
For obese subjects, including those with the metabolic syndrome, weight loss is
a cornerstone of therapy, not only by reducing AHI ( apnea-hypopnic index
- the number of obstructive events per hour), though seldom to
normal, but also by improving hypertension, lipid metabolism, and insulin
resistance. Patients with a normal BMI, severe OSA at diagnosis, or those
having difficulty losing weight require specific treatment of OSA, such
as nasal CPAP or an oral appliance. The mainstay of OSA therapy for the
past 20 years has been nasal CPAP. But an alternative or even first line treatment of mild and moderate OSA is the use of oral appliance therapy, which can also serve as therapy for severe OSA, where CPAP is not viable or tolerable (Personal communication from Dr. David J. Stern DDS, DABDSM, MSCC, MAAD, Member of Canadian Sleep Society).
As you are probably aware of the most recent guidelines, in the practice parameters established by the AASM has recomended Oral Appliance Therapy as a first line treatment of Mild and Moderate OSA and even as therapy for Severe OSA where Cpap is is not viable or tolerable. I sincerely believe your readers may benefit from this information and may be appreciative aware of more alternatives to treatment.
Kindest regards
David Stern
DR. DAVID J. STERN DDS, DABDSM ,MCSS,MAAD
Doctor of Dental Surgery
Diplomate of The American Board of Dental Sleep Medicine
Member of The Canadian Sleep Society
Member of The American Academy of Cosmetic Dentistry
1. The most commonly prescribed treatment
for obstructive sleep apnea is
continuous positive airway pressure (CPAP). The CPAP machine
delivers
air pressure through a small nasal mask that the patient wears
while
sleeping (osa-fig7).
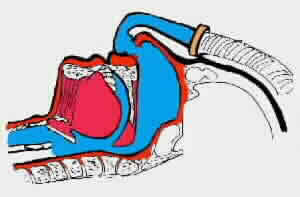
Figure 7: CPAP flow generators develop a constant,
controllable pressure to keep the upper airway open so that
one can breath normally. CPAP is effective on 95% of the patients
with OSA. The units are reliable, quiet and efficient and come
in a variety of sizes and shapes.
Controlled pressure is induced through the nasal passage, holding
the soft tissue of the uvula and soft palate and the soft pharyngeal
tissue in the upper airway in position so the airway remains
open while one descends into the deeper stages of sleep and
REM sleep. The pressure acts much in the same way as a splint,
holding the airway open.
The pressure acts as an "air splint"
as noted above ,which keeps the
throat open ,eliminating obstructive apneas and allowing one
to breathe normally all night long. Sleep becomes uninterrupted
and restorative. For many
patients, CPAP therapy dramatically improves their daytime functioning
as well as their general health. CPAP is not a cure, but a noninvasive
therapy for managing OSA.
There are typically three methods of inducing
the pressure and airflow into the nasal cavity: nasal masks,
nasal pillows and nasal seals. The most common used is the nasal
mask. Nearly all CPAP manufactures make at least one style of
nasal mask, most make two or three different ones. Nasal pillows
are small, oval shaped latex rubber prongs that fit into the
opening of the nostril. They are held in place by a shell that
is attached to the headgear. When fit properly they are very
comfortable and seldom leak. Nasal seals fit against the opening
of the nostril and are held in place by a special frame attached
to the headgear.
Compliance can be a problem, even in patients
with severe symptomatic
OSA. some patients do not tolerate the therapy, and others find
purchasing a machine financially prohibitive.Early followup
when commencing CPAP therapy is important.Common concerns raised
when initiating CPAP therapy include nasal congestion or dryness,which
can usually be over come with a humidifier,and abrasions or
mask leak,which respond to local measures.
Nursing support and intensive education programs
have also been shown to improve compliance.Followup studies
indicate,on the average,4 h of effective CPAP is administered
per night,and even thie amount of CPAP treatment improves daytime
tiredness.
The latest development in CPAP treatment is
automated CPAP.These devices determine the prssure for each
breath.Improved tolerability is particularly noticeable in patients
who awake frequently,those with body dependent and rapid eye
movement-related OSA.Detailed data logging of compliance and
air l=eak by these devices also allows monitoring of the effectiveness
of the treatment.
2. Sleep apnea can also be treated surgically.
However, the costs and
success rates may vary greatly depending on which procedure
is chosen
and the experience and skills of the surgeons. If one wishes
to consider
surgical treatment of OSA, learning as much as one can about
the various
surgical procedures is very highly recommended. One must also
be certain
the surgeons are well qualified and have successfully treated
many patients.
3. The following surgical procedures are available
foe OSA in patients who cannot tolerate CPAP.Caution is necessary
when prescribing these therapies,as apneas are rarely completely
averted and less information is available on their effectiveness,particularly
in patients with cardiac failure:
Genioglossus Tongue Advancement
Hyoid Suspension
Somnoplasty (Radio frequency or RF procedure)
Maxillomandibular Advancement


osa-fig. 6I and 6J Lateral skull radiographs
of a patient before and after treatment.
(Lower) The patient
has a retruding jaw and an attenuated posterior airway space
of 6 mm (arrows).
(Upper) Maxillofacial surgery produces normal
maxillary-mandibular occlusion and an adequate posterior airway
diameter of 12 mm (arrows).
Laser Assisted Uvuloplasty (LAUP)
Uvulopalatopharyngoplasty (UPPP)
Tracheostomy,in extreme situations where OSA is severe and CPAP
is not tolerated.
4. Finally, some patients try dental appliances.
These appliances work by
bringing the lower jaw forward to increase the size of the airway.
This
approach is usually reserved for milder cases of OSA or for
individuals
who snore but don't obstruct. Relatively few well-designed studies
exist
to show that these appliances work well, nor has patient compliance
been
carefully evaluated.
How does Continuous Positive Airway
Pressure (CPAP) therapy work?
In the last decade and a half, continuous
positive airway pressure
(CPAP) machines have been the most effective way of treating
obstructive
sleep apnea.
1. To use the machine, a small comfortable
mask is fitted over
the nose leaving the mouth uncovered. Patients must sleep with
their
mouths closed, aided by a chin strap, while the machine gently
blows air
into the nose at a pressure slightly higher than the surrounding
air
pressure. Most people get used to it quickly, some do not.
2. Literally within minutes of achieving the
correct CPAP pressure to
maintain an open airway, patients with obstructive sleep apnea
start
sleeping like people who have gone without sleep for many days.
For the
first week or so after starting to use the machine, patients
will spend
a great deal of time in deep sleep. Patients often report that
there is
a dramatic increase of daytime alertness and energy in just
a few nights
on CPAP.
3. Nasal CPAP is by now a very well established
and safe treatment. Most
insurance companies will cover the cost of leasing or purchasing
a
machine. Today, thousands of CPAP users are now happy after
experiencing
a dramatic positive improvement in their daytime alertness and
energy level.
There are three types of CPAP devices: Standard
CPAP, Bi-level CPAP, and
Smart CPAP.
Who To Treat?
Treatment of OSA to relieve symptoms of daytime
tiredness and to avoid somnolence-induced motor vehicle and
work-related accidents is an established practice . Recently
there has been increased interest in the role of CPAP to prevent
cardiovascular disease and aid in controlling hypertension.
Evidence for a dose-response relationship between AHI and daytime
hypertension is strong, and small studies have shown improvements
in blood pressure , baroreceptor sensitivity , and nitric oxide
derivative production , and a reduction in sympathetic nervous
system activation with treatment of OSA.
In heart failure patients, CPAP provides symptomatic relief
and reduces the need for incubation during acute exacerbations
. Small trials have demonstrated improved quality of life and
exercise capacity with CPAP therapy. Improved left ventricular
ejection fraction has also beenIn heart failure patients, CPAP
provides symptomatic relief and reduces the need for intubation
during acute exacerbations . Small trials have demonstrated
improved quality of life and exercise capacity with CPAP therapy.
Improved left ventricular ejection fraction has also been reported,
with deterioration in left ventricular ejection fraction on
withdrawal of therapy . Mechanisms by which CPAP therapy exerts
its beneficial effect may include reductions in left ventricular
afterload and sympathetic nerve activity . Currently, the Canadian
Continuous Positive Airway Pressure Trial for Congestive Heart
FailurePatients with Central Sleep Apnea (CANPAP) is underway,
with the aim of further defining the role of CPAP in heart failure
therapy .
Arrhythmia reduction and improved PHT have also been reported
with CPAP. For many cardiovascular events, including acute coronary
syndromes and sudden death, however, no treatment studies are
available, so treatment decisions must be made empirically.
Figures osa 1, 2, 3, 4 from Lattimore, Jo-Dee
L. and al. OSA and Cardiovascular Disease, Jaccvol.41, No.9.2003, May , 2003: 1429-37.
Figures osa 6D, 6F,6I, 6J from Sheldon Mintz,
D.D.S., M.S., M.S., Dearborn, Mich.
Figures osa 6c, 6e from Lyle D. Victor, M.D., Department of
Medical Education, Oakwood Hospital, 18101 Oakwood Blvd., Dearborn,
MI 48124