DISORDERS ON THE CARDIOVASCULAR SYSTEM
Dominique L Musselman / William McDonald
/ Charles B. Nemeroff
"And now here's my secret, a very simple secret: It is
only with
the heart that one can see rightly; what is essential is invisible
to
the eye.
(Antoine de Saint-Exupery, The Little
Prince, 1943)"
INTRODUCTION: DEPRESSION
AND COMORBID MEDICAL ILLNESS
The interactions of personality traits, psychiatric symptoms
and syndromes, and environmental stressors with the cardiovascular
system have long intrigued investigators interested in the factors
that
contribute to the development and progression of atherosclerotic
heart disease. Differences in rates of ischemic heart disease
(IHD)
remain substantially unexplained even after surveillance of
the
well-established risk factors. Although the type A personality
pattern has been studied intensely as a risk factor for coronary
artery
disease (CAD), lack of a consistent association between type
A behavior and the subsequent development of IHD has stimulated
questions about the
contributions of the psychological concept of hostility as well
as the
syndrome of major depression. Increasing evidence is accumulating
suggesting that major depression (Table 1 below) a mood disorder,
is
associated with drastically elevated morbidity and mortality
after an index
myocardial infarction (MI) and also acts as an independent risk
factor
in the development of atherosclerotic heart disease.
Depressive syndromes and major depression are exceedingly common.
The most recent comprehensive study done in the United States,
the National Comorbidity Study, reported life-time prevalence
rates of major depression and dysthymia of 13 percent and 5
percent, respectively.4 Point prevalence rates of major depression
in primary care outpatients range from 2 to 16 percent and 9
to 20 percent for all depressive disorders and are even higher
among medical inpatients: 8 percent for major depression and
15 to 36 percent for all depressive disorders.
Minor depressive disorder (depressive symptoms subthreshold
in severity
compared with major depression and dysthymia) is also common
in the
community and in primary care clinics. The Epidemiologic Catchment
Area Study of over 18,500 individuals reported the lifetime
prevalence rate of sub-threshold depressive symptoms to be 23
percent in comparison to 6 percent, the sum of the prevalence
rates of major depression and dysthymia. Although depression
in patients with CAD is diagnosed infrequently by primary care
physicians and
cardiologists, recognition and treatment of major depression
is crucial,
especially for patients after an MI. Not only do depressed patients
experience great difficulties in problem solving and coping
with challenges,
depression adversely effects compliance with medical therapy
and
rehabilitation and increases medical comorbidity. Minor depressive
disorder also is associated with significant functional impairment
and substantial increases in health care utilization.
In patients with CAD, depression predicts future cardiac events
and
hastens mortality. Since the 1960s, multiple cross-sectional
and
longitudinal studies have scrutinized the association of cardiovascular
disease (CVD), especially CAD and congestive heart failure (CHF),
with depressive sympthms is well as major depression.
|
TABLE 1 DSM-IV
Diagnostic Criteria tor Depressive Disorders
MAJOR DEPRESSIVE DISORDER
A. Five or more of the following symptoms have been present
during the same 2-week period and represent a change from
previous functioning; at
least one of the symptoms is either (1) depressed mood
or (2) loss of interest or pleasure.
1. Depressed mood
2. Markedly diminished interest or pleasure
3. Significant weight loss or weight gain or decrease
or increase in
appetite
4. Insomnia or hypersomnia
5. Psychomotor agitation or retardation (observable by
others)
6. Fatigue or loss of energy nearly every day
7. Feelings of worthlessness or excessive or inappropriate
guilt
8. Diminished concentration or indecisiveness
9. Recurrent thoughts of death (not just fear of dying)
or suicide
B. The symptoms cause clinically significant
distress or impairment in
social, occupation, or other important areas of functioning.
C. The symptoms are not due to the direct physiologic
effects of a
substance or a general medical condition.
D. The symptoms are not better accounted for by bereavement.
DYSTHYMIC DISORDER
A. Depressed mood for most of the day, for more days than
not, for at
least 2 years
B. Presence, while depressed, of two
or more of the following:
1. Poor appetite or overeating
2. Insomnia or hypersomnia
3. Low energy or fatigue
4. Low self-esteem
5. Poor concentration or difficulty making decisions
6. Feelings of hopelessness
C. The disturbance is not better accounted for by a chronic
major
depressive disorder.
Diagnostic and Statistical
Manual of Mental Disorders, 4th ed. Copyright 1994, American
Psychiatric Association.
|
EPIDEMIOLOGY
Depression and CardiovascuLar Disease
Early studies reported the prevalence of depression to be 18
to 60
percent in patients with CAD. Later studies reported relatively
consistent prevalence rates of depression in patients with CVD
(patients with CAD) ranging from 16 to 23 percent (mean, 19
percent; median,18 percent) despite the potential methodologic
weaknesses of some of the studies listed in Table
2 (such as the use of unmodified psychiatric diagnostic
instruments to determine the prevalence of depression, excluding
patients
because of the severity of CVD, and measuring depressive symptoms
at differenttimes after hospital admission) and methodologic
differences among
the studies (dissimilar patient populations, different diagnostic
instruments, different hospitalization status, unspecified type
of heart
disease).
Although the prevalence of major depressive symptoms in patients
hospitalized for CHF has not been as well studied, preliminary
evidence indicates that these patients have equally high or
even higher
rates of major depression.37'39 However, although severity of
physical
illness is one of the most important variables associated with
depression in
patients with other medical illnesses, studies of patients with
CVD do
not always document a higher prevalence rate of depression in
patients
with measures of more advanced CVD or a greater level of
disability.
Depression as a Risk Factor
for Ischemic Heart Disease
The notion that having a psychiatric illness such as major
depression increases one's risk for developing ischemic heart
disease remains controversial and often has been "explained"
intuitively by the hypothesis that persons with psychiatric
disorders generally have
other risk factors for the development of CAD. 1 Table 80-3
describes the
studies with the most rigorous methods:Those studies have been
prospective in design, have used structured clinical interviews
or diagnostic instruments, have included other risk factors
for CVD in their analyses (such as hypertension,
hypercholesterolemia, nicotine and other substance abuse, and
physical inactivity), and have been controlled for demographic
factors (such as age, sex, and socioeconomic status).Nearly
all the recent studies in Table 3 document increased cardiovascular
morbidity and mortality in patients with depressive symptoms
or major depression, implicating depression as an independent
risk factor in the pathophysiologic progression of CVD rather
than merely as a secondary emotional response to cardiovascular
illness.Such large epidemiologic studies may use self-report
instruments ratherthan clinical interviews to evaluate the importance
of psychological factors in predicting CVD. Assessments of this
type typically are added to large, multiple-risk-factor studies
in which population-based samples are followed up prospectively.'
The advantage of using "dimensional" measures of depression
(rather than a categorical diagnosis of major depression) lies
in the increased statistical power that allowsthese studies
to detect smaller "effects." However, such epidemiologic
data are not equivalent to clinical data. A relatively large
clinicalstudy supporting depression as an independent risk factor
for CVD
observed hat patients with major depression experienced elevated
mortality rates after an MI. Frasure-Smith and colleagues found
depression to be a
significant predictor of mortality (p < .001) in 222 patients
6
months after an MI. Depression remained a significant predictor
of
mortality (p = .01) even after multivariate statistical methodology
was used to factor out the effects of left ventricular dysfunction
and previous
MI. Multiple logistic regression analyses revealed that depression
was
significantly related to 18-month cardiac mortality even after
controlling for other significant multivanate predictors of
mortality
(previous MI,,Killip class frequency of permature ventricular
contractions(Pvcs)(p=.003).
TABLE 2. Prevalence of Major Depression
in Patients with
Cardiovascular Disease
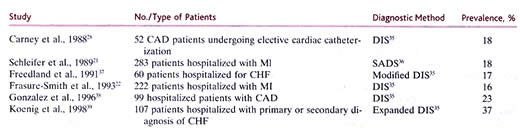
ABBREVATIONS:
CAD = coronary artery disease; MI = myocardial infarction; DIS
= Diagnostic Interview Schedule, Version III; SADS = Schedule
for Affective Disorders and Schizophrenia.
SOURCE:
Adapted from and reprinted with permission from Archives of
General Psychiatry 55:580--592, July 1998. Copyrighted 1998,
American Medical Association.
PATHOPHYSIOLOGY
Hypothalamic-Pituitary-Adrenocortical
and SympathomeduLLary Hyperactivity
Recent advances in biological psychiatry have included the discovery
of numerous neurochemical, neuroendocrine, and neuroanatomic
alterations in unipolar depression. Often proposed as important
adjuncts in the diagnosis of depressed subjects, some of these
biological markers may reflect important pathophysiologic alterations
that contribute to the increased vulnerability of depressed
patients to CVD. These markers include sympathoadrenal hyperactivity,
diminished heart rate variability (HRV), alterations in platelet
receptors and/or reactivity, and ventricular instability and
myocardial ischemia in reaction to mental stress (Fig.
208).
Two primary components that are central to the "fight or
flight" stress response observed by Cannon in and the "general
adaptation syndrome" described by Selye in 195663 are the
hypothalamic-pituitary-adrenocortical axis and the sympathoadrenal
system. In response to stress, hypothalamic neurons containing
corticotropin-releasing factor (CRF) increase the synthesis
and release of corticotropin (ACTH), /3-endorphin, and other
pro-opiomelanocortin (POMC) products from the anterior pituitary
gland. Many studies have documented evidence of hypothalamic-pituitary-adrenocortical
axis hyperactivity in medication-free patients with major depression,i.e.,
elevated CRF concentrations in cerebrospinal fluid, blunting
of the ACTH response to CRF administration, nonsuppression of
cortisol
secretion after dexamethasone administration, hypercortisolemia,
and
pituitary and adrenal gland enlargement, as well as direct evidence
of increased numbers of hypothalamic CRF neurons in postmortem
brain tissue from depressed patients compared with controls.
Administered corticosteroids have long been known to induce
hyperdholesterolemia, hypertriglyceridemia, and hypertension.
Other atherosclerosis-inducing actions of steroids include injury
to vascular endothelial cells and intima and the inhibition
of normal healing. Indeed, elevated morning plasma cortisol
concentrations have been significantly correlated with moderate
to severe coronary atherosclerosis in young and middle-aged
men.
Many patients with major depression also exhibit dysregulation
of
the sympathoadrenal system. The adrenal medulla and sympathetic
nervous
system (SNS) together constitute the sympathoadrenal system.
Although central nervous system (CNS) regulation of the sympathoadrenal
system has been only partially characterized, hypothalamic CRF-containing
neurons provide stimulatory input to several autonomic centers
that
are involved in regulating sympathetic activity. Nerve impulses
from
regulatory centers in the CNS control catecholamine release
from the
sympathoadrenal system. Physiologic and pathologic conditions
causing sympathoadrenal activation include physical activity,
coronary
artery ischemia, heart failure, and mental stress. Epinephrine
in plasma
is derived from the adrenal medulla, whereas plasma norepinephrine
(NE) concentrations reflect the secretion of NE largely from
sympathetic
nerve terminals, with the remaining NE provided by the adrenal
medulla
and extraadrenal chromaffin cells. Peripheral plasma NE concentrations
are determined not only by the rate of release from sympathetic
system nerve terminals but also by reuptake into presynaptic
terminals, local metabolic degradation, and redistribution into
multiple
physiologic compartments. Hypersecretion of NE in unipolar
depression has been documented by elevated plasma NE and NE
metabolite
concentrations and elevated urinary concentrations of NE and
its
metabolites. Not only do depressed patients exhibit higher basal
plasma concentrations of NE. those with melancholia exhibit
even greater
elevations in plasma NE concentrations when subjected to orthostatic
challenge than do normal control subjects and depressed patients
without melancholia.n Furthermore, depressed patients who are
dexamethasone (DST) nonsuppressors exhibit significantly higher
basal and
cold-stimulated plasma concentrations of NE than do depressed
patients who are DST suppressors. After treatment with tricyclic
antidepressants (TCAs), urinary excretion of NE and its metabolites
diminishes together with plasma NEconcentrations,although Veith
and colleagues reported that chronic treatment with desipramine
increased plasma concentrations of NE.Thus,sympathoadrenal hyperactivityy
seems to represents a state rather than a state rather than
a state or trait marker of depression, possibly reflecting increased
CRF release within the CNS.
Sympathoadrenal hyperactivity contributes to the development
of CVD
through effects of catecholamines on the heart, blood vessels,
and
platelets. Sympathoadrenal activation modifies the function
of
circulating platelets through direct effects on platelets,
catecholamine-induced changes in hemodynamic factors (increased
shear stress), circulating lipids, and inhibition of vascular
eicosanoid
synthesis Arachidonic acid metabolites such as prostaglandins
and
leukotrienes contribute to diverse circulatory and hemostatic
functions,including inhibition of platelet aggregation, and
vascular
contractility and permeability. Elevations of plasma NE levels
are found most frequently in young hypertensive patients and
in subjects with
high-cardiac-output borderline hypertension who later proceed
to
established high-resistance hypertension.95 Even normotensive
depressed after orthostasis, and after exercise in comparison
with normal controls.
These depressed patients also exhibited increased plasma
concentrations of NE and serotonin (5HT) at restThus the sympathoadrenal
hvoeractivity observed in trait marker of depression, possibly
reflecting increased CRF release > within the CNS.
Sympathoadrenal hyperactivity contributes to the development
of CVD
through effects of catecholamines on the heart, blood vessels,
and
platelets. Sympathoadrenal activation modifies the function
of
circulating platelets through direct effects on platelets,
catecholamine-induced changes in hemodynamic factors (increased
shear stress), circulating lipids, and inhibition of vascular
eicosanoid
synthesis Arachidonic acid metabolites such as prostaglandins
and
leukotrienes contribute to diverse circulatory and hemostatic
functions, including inhibition of platelet aggregation, and
vascular
contractility and permeability.93 Elevations of plasma NE levels
are found most frequently in young hypertensive patients and
in subjects with
high-cardiac-output borderline hypertension who later proceed
to > established high-resistance hypertension.95 Even normotensive
depressed patients have been found to exhibit greater heart
rates at rest,
after orthostasis, and after exercise in comparison with normal
controls.
These depressed patients also exhibited increased plasma concentrations
of NE and serotonin (5HT) at rest. Thus the sympathoadrenal
hvoeractivity observed in many patients with major depression
may contribute to the development of CVD through the effects
of catecholamines on cardiac function and platelets.
Diminished Heart Rate Variability
Alterations in autonomic nervous system activity, as demonstrated
by reduced HRV, represent another mechanism that potentially
contributes to the diminished survival of depressed patients
with CVD. It is
believed that the beat-to-beat fluctuations in hemodynamic parameters
reflect the dynamic response of cardiovascular control systems
to a myriad of naturally occurring physiologic perturbations,
such as fluctuations in heart rate associated with respiration.
Therefore, HRV may providea sensitive measure of the functioning
of the rapidly reacting sympathetic, parasympathetic, and renin-angiotensin
systems.
Cardiovascular homeostasis is maintained by the parasympathetic
and
sympathetic nervous systems through afferent pressor receptors
and
chemoreceptors and efferents that alter heart receptors and
efferents that alter heart rate,atrioventricular conduction,and
contractility and impinge on the peripheral vasculature,altering
arterial and venous vasomotor tone.HRV is the standard deviation
of successive R-R intervals in sinus rhythm and reflects the
interplay and balance between sympathetic and parasympathetic
input on the cardiac pacemaker. Peripheral control of HRV occurs
mainly through the parasympathetic cholinergic vagus nerve Central
generation and control of heart rate are regulated by the hypothalamus,
the limbic system, and the brainstem. Numerous CNS neurotransmitters
are involved in modulating HRV, including acetylcholine, NE,
5HT, and dopamine.
A high degree of HRV is observed in normal hearts with good
cardiac function, whereas HRV can be decreased significantly
in patients with severe CAD or heart failure. Moreover, the
relative risk of sudden death after an acute MI is significantly
higher in patients with decreased HRV. Heart rate variability
is one of many prognostic factors after an infarction age, left
ventricular ejection fraction (LVEF), and frequency of arrythmias.
Its positive predictive power, like that of other factors after
an MI, is relatively modest when considered in isolation. Although
positive predictive accuracy is not high when HRV is considered
in combination with other prognostic factors, clinically useful
levels of negative predictive accuracy can be achieved. Among
the many arrhythmogenic factors, autonomic tone is the most
difficult to measure, and therefore, interest in HRV continues.
Power spectral analysis measurements of HRV often are used because
certain frequency bands of the heart period power spectrum have
been associated with autonomic nervous system control of the
sinus node.The low-frequency power of the heart period power
spectrum reflects modulation of sympathetic and vagal tone by
baroreflex activity. while high-frequency power reflects modulation
of vagal tone, primarily by respiratory frequency and depth,
i.e., respiratory sinus arrhythmia. The physiologic mechanisms
that contribute to ultralow-frequency and very low frequency
power of the heart period spectrum (which account for more than
90 percent of the total power in a 24-h period) remain obscure.
In a study of 715 patients after Ml, certain frequency bands
(total, ultralow, and very low frequencies) of the heart period
power spectrum were strongly associated with mortality during
4 years of follow-up even after adjustment for other major risk
factors. Indeed, very low frequency power was most strongly
associated with death secondary to arrhythmia.
Reduced high-frequency HRV has been observed in depressed patients
in comparison with nondepressed groups, although discrepant
reports exist. In patients with angiographicalI~ confirmed CAD,
diminished HRV during 24-h Holter monitoring was significantly
more common in depressed patients than in matched nondepressed
patients)21 Diminished high-frequency HRV is thought to reflect
decreased parasympathetic tone, possibly predisposing patients
to ventricular arrhythmias and perhaps to the excessive cardiovascular
mortality found in CVD patients with a comorhid major depressive
disorder Diminished HRV in patients with major depression also
may be contributed to by a deficiency of omega-3 fatty acids'23
in this patient population. Not only have multiple studies documented
a deficiency of omega-3 fatty acids in patients with major depression)
1 these polyunsaturated lipids possess antiarrhvthmic properties
and reduce the risk of ventricular arrhythmias.
One study (without a placebo control group) revealed normalization
of reduced HRV in depressed patients after effective treatnient.
The prognostic importance of antidepressant-in-duced improvement
in diminished HRV in depressed patients remains an intriguing
area of research. Subsequent investigations will seek to determine
the processes that underlie ultralow and very low frequency
bands of the heart power spectrum; whether these bands are altered
in depressed patients (with or without CVD) remains obscure.
Alterations in Platelet Receptors
and/or Reactivity
The adverse effects of depression on cardiovascular
disease also may be mediated by platelet mechanisms. Markovitz
and Matthews's' first proposed that enhanced platelet responses
to psychologic stress may trigger adverse coronary artery ischemic
events. This association between platelet activation and vascular
disease is supported indirectly by studies linking cerebrovascular
disease and depression. The Established Populations for Epidemiologic
Studies of the Elderly prospectively studied 10,294 persons
age 65 and older for 6 years and determined that rates of stroke
(adjusted for age, physical disability, and other medical disorders)
were 2.3 to 2.7 times higher in persons designated with 'high"
versus 'Slow" levels of depressive symptoms. In another
prospective study, 103 consecutive stroke patients were assessed
for major depression or dysthymia approximately 2 weeks after
a stroke. Patients with major depression or dysthymia were 3.4
times more likely to have died during the 10-year follow-up
period than were nondepressed patients (p = .007) even after
controlling for confounding variables (age, medical comorbidity,
type of stroke, and lesion location) (p = .03).
Platelets play a central role in hemostasis, thrombosis, the
development of atherosclerosis, and acute coronary syndromes'36
through their interactions with both subendothelial components
of damaged vessel walls and plasma coagulation factors, primarily
thrombin. Human platelets contain adrenergic, serotonergic,
and dopaminergic receptors. Through activation of platelet alpha2
adrenoceptors, increases in circulating catecholamines (>4
nmol/L) potentiate the effects of other agonists and, at higher
concentrations, initiate platelet thrombotic responses, including
secretion, aggregation, and activation of the arachidonate pathway.
After injury to vessel endothehum, platelets and circulating
leukocytes attach to the newly exposed subendothelial layer.
Platelets adhere to collagen (and other components of the subendothelial
matrix) exposed within a denuded area of the vascular endothelium.
Thrombin stimulates platelet activation, converting platelet
membrane GPIIb/ lila complexes into functional receptors for
fibrinogen. Activation also is accompanied by extrusion or secretion
of platelet storage granule contents into the extracellular
environment. Platelets activated at the site of an injury to
the vessel wall accelerate the local formation of thrombin and
release a variety of products from their storage granules, including
chemotactic and mitogenic factors, inducing leukocyte migration
from the bloodstream and vascular cell proliferation. These
secreted platelet products, e.g., platelet factor 4, /3-thromboglobulin
(f3-TG), and 5HT, stimulate and recruit other platelets and
cause irreversible platelet-platelet aggregation, ultimately
leading to the formation of a fused platelet thrombus. Platelets
also contribute to vascular damage by stimulating lipoprotein
uptake by macrophages and mediating vasoconstriction through
the production and/or release of substances such as thromboxane
A, platelet-activating factor, and 5HT. Clinical trials have
conflrmecl the importance ot platelets in vascular damage ;antiaggregating
medications are useful in secondary prevention, delay the progression
of atherosclerotic lesions, and improve post-MI outcomes.
The authors sought to determine whether heightened
susceptibility to platelet activation might be a mechanism by
which depression in physically healthy young volunteers acts
as a significant risk factor for cardiovascular and cerebrovascular
disease and/or increased mortality after MI. Utilizing fluorescence-
activated flow cytometric analysis, the authors discovered that
in comparison with 8 normal controls, 12 depressed patients
as
a group exhibited enhanced baseline platelet activation as well
as increased platelet responsiveness.
In one study, 21 elderly patients suffering
from comorbid s
CVD and major depression exhibited increased platelet activation
as measured by markedly elevated plasma concentrations of the
platelet secretion products PF4 and beta-TG compared with 17
healthy control subjects and 8 nondepressed age-matched patients
with CVD. Although the mechanism or mechanisms responsible remain
unknown, the authors believe that heightened susceptibility
to platelet activation and secretion underlies, at least in
part, the increased vulnerability of depressed patients to CVD
and/or mortality after an MI.
Serotonin secreted by platelets induces both platelet aggregation
and coronary vasoconstriction, both of which are mediated by
5HT2 receptors. Vasoconstriction occurs especially when normal
endothelial cell counterregulatory mechanisms of vascular relaxation
are defective, as often occurs in patients with CAD. Indeed,
essential hypertension, elevated plasma ,cholesterol levels,
older age, and smoking, which are well- known predisposing factors
for the development of CVD, all contribute to 5HT-mediated platelet
activation. Moreover, alterations in platelet 5HT-mediated activation
also have been described in affective disorders, most notably
major depression.
Considerable evidence has accrued in the last two decades that
supports the hypothesis that alterations in CNS and platelet
serotonergic function occur in depressed patients.
Serotonin-mediated platelet activation can
contribute to the
development of atherosclerosis, thrombosis, and vasoconstriction.
Even though 5HT is a weak platelet agonist, it markedly amplifies
platelet reactions to a variety of other agonists such as adenosine
diphosphate (ADP), thromboxane A2, catecholamines, and thrombin.
Through an action on 5HT2 receptors,serotonin enhances platelet
aggregation and the release of intragranular products and arachidonic
acid metabolites in response to otherwise ineffective agonist
concentrations. This 5HT induced platelet amplification occurs
at the low concentrations attained when indoleamine is released
from seeping platelets subjected to shear stresses and from
platelet activation by contact with an arterial wall lesion.
Several investigators have reported increases in platelet 5HT2
binding density in depressed patients. Moreover, the changes
appear to be state-dependent in that 5HT2 binding-site density
returned to control values only in patients who showed clinical
improvement. Depressed patients have been found to exhibit significant
reduction in the number of platelet and brain 5HT transporter
sites as detected by [S3H] imipramine binding as well as by
the more selective ligand (3H] paroxetine.The increased 5HT2
creceptor binding density and decreased 5HT transporter sites
suggest that depressed patients may be particularly susceptible
to 5HT-mediated platelet activation and coronary artery vaso-constriction.
Decreased numbers of platelet 5HT transporters would potentially
hinder the uptake and storage of periplatelet serotonin, exposing
the increased numbers of 5HT2 receptors to 5HT.
Platelets from depressed patients exhibit significantly increased
elevations of intracellular free calcium concentration, (Ca2+)i
after 5HT-induced stimulation in comparison to controls. Even
functionally trivial increases in intraplatelet calcium "prime"
the platelet secretion and aggregation response to stimulation
by even a "weak" agonist such as 5HT or in response
to increased blood flow. Thus, platelets with elevated (Ca2+)i
as are observed in depressed patients, probably would exhibit
increased activation in comparison with normal comparison subjects
under basal conditions or in response to shear-induced aggregation
(e.g., after an orthostatic challenge). Future investigations
will attempt to confirm and connect the pathophysiologic mechanisms
of sympathoadrenal hyperactivity, exaggerated platelet reactivity,
and alterations in the platelet 5HT system in depressed patients
to the propensity of those patients for the development of CVD.
Myocardial lschemia and Ventricular
Instability in Reaction to Mental Stress
The combination of a vulnerable myocardium after MI, acute ischemia,
and negative emotional arousal is thought to trigger fatal ventricular
arrythmias. The interplay of these factors in patients with
CAD is being scrutinized. Jiang and colleagues longitudinally
assessed 126 patients with CAD over a 5-year period. Mental
stress-induced myocardial ischemia at baseline in CAD patients
was associated with significantly higher rates of subsequent
fatal and nonfatal cardiac events independently of age, baseline
LVEF, and previous Ml. This study proposed that the relation
between psychological stress and adverse cardiac events is mediated
by myocardial ischemia. Although myocardial ischemia probably
is the most significant factor in predisposition to ventricular
instability, other factors also contribute. CNS control mechanisms
can significantly decrease the threshold for ventricular fibrillation.
Ventricular fibrillation is believed to be the mechanism underlying
sudden cardiac death, the most common cause of fatality among
patients with CAD. Indeed, psychological stress predisposes
to abnormal ventricular activity by lowering the ventricular
vulnerable-period threshold even to the point of fibrillation.
The vagus nerve, however, exerts antiarrthymic activity through
a direct action on the ventricular myocardium and interference
with sympathetic activity. Increased parasympathetic activity
has a protective effect on myocardium electrically destabilized
by increased adrenergic tone.
Psychological and physical events can elicit a stress response,
which usually is defined as the reaction of an organism to deleterious
forces that disturb physiologic homeostasis. Psychological stress
in humans with CAD increases ventricular ectopic activity and
increases the risk of ventricular fibrillation. There are several
similarities between the stress response and major depression:
both can be characterized by increased blood pressure and heart
rate as well as increased arousal and increased mobilization
of energy stores.Particularly relevant to both the stress response
and depression are the criticalbrain structures the locus coeruleus
and the central nucleus of the amuygdala,which both are innervated
by CRF-containing nerve terminals. The stress response and major
depression differ in some respects, however. In depression,
some aspects of the normal stress response seem to escalate
to a pathologic state'78 that fails to respond appropriately
to usual counterregulatory responses, resulting in a sustained
version of a usually transient phenomenon, i.e., hyperactivity
of the hypothalamic-pituitaryadrenocortical (HPA) axis or the
sympathoadrenal system. Although many studies have linked stressful
life events to the onset of major depression, some depressions
are clearly endogeneous-i.e., they have no obvious environmental
precipitant-although in most of these studies the role of early
adverse events that are now known to be of paramount importance
was not assessed.
Frasure-Smith and colleagues proposed that
depression worsens the prognosis after an MI through another
mechanism:
PVCs. The risk of sudden cardiac death associated with significant
depressive symptoms (Beck Depression Inventory score approximately
10) was greatest among patients with 10 or more PVCs per hour
(60 percent of these patients died within 18 months), suggesting
arrythymia as the link between depression and sudden cardiac
death. Depressed patients with CAD are not more likely to have
arrhythmias than are nondepressed patients with CAD, but the
risk associated with depression is confined largely to patients
with PVCs. Patients who were not depressed experienced little
increase in risk associated with PVCs even in the presence of
a low LVEF. Thus, the prognostic impact of PVCs may be related
more to depression than to PVCs per se. In the Cardiac Arrhythmia
Suppression Trial (CAST), suppression of PVC frequency in post-MI
patients did not reduce but actually increased mortality even
though PVCs are associated with increased mortality after an
MI. Treatment of depression may be necessary to improve survival
in depressed patients with PVCs.
ANXIETY DISORDERS AND CARDIOVASCULAR
DISEASE
Epidemiology
Anxiety disorders are the most prevalent psychiatric
disorders in the United States (Table 4), with simple phobias
being the most common (9 percent) and social phobia (8 percent)
being the most often observed (Tables -5 and -6). A survey of
adult primary care patients (n = 637) enrolled in a health maintenance
organization revealed that 10 percent had untreated anxiety
disorders.
TABLE 4 12-Month Prevalence of DSM-IH-R Disorders in the National
Comorbidity Survey
Disorder ---------------------------------------Percent
Any anxiety disorder --------------------------19.3
Any addictive disorder ------------------------11.3
Any mood disorder ----------------------------11.3
Nonaffective psychosis -----------------------0.3
Any National Cornorbidity, Survey disorder-30.9
TABLE 3 Antecedent Depression and Subsequent
Risk of Cardiovascular Disease
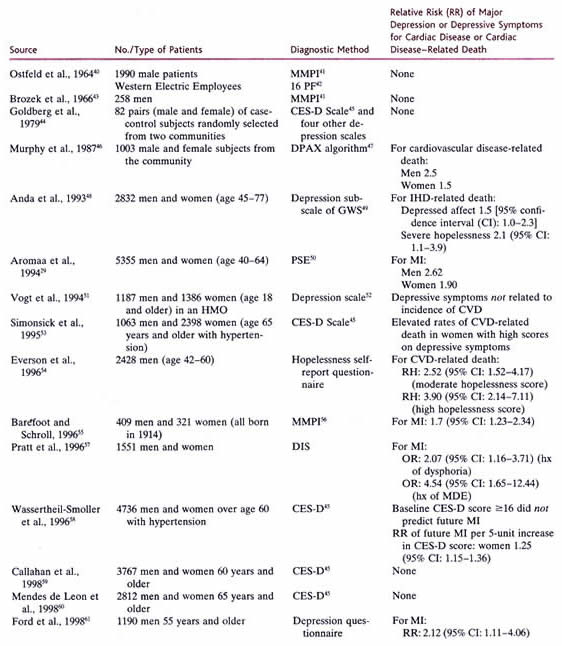
ABBREVIATIONS:
RH = relative hazard; IHD = ischemic heart disease; MI = myocardial
infarction; hx = history; MDE = episode of major depression;
OR = odds ratio; CI = confidence interval.
SOURCE:
Adapted from and reprinted with permission from Archives of
General Medical Association.
The Relationship Between Major Depression
and Cardiovascular Disease
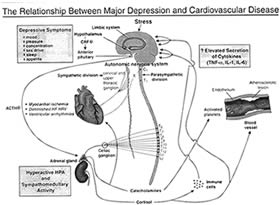
Fig.208
click to enlarge
Hypothetical schema of pathophysiologic
findings is shown. CRF = corticotropin-releasing factor; ACTH
= corticotropin; associated with depression that probably contribute
to increased susceptibility TNF-a = tumor necrosis factor a;
IL-i =interleukin-1;IL-6 = interleukin-6; to cardiovascular
disease. Autonomic nervous system innervation of the heart HRV
= heart rate variability; HPA =hypothalamic-pituitary-adrenocortical
via the parasympathetic vagus (X) nerve and sympathetic (postgangtionic
axis. efferents from the cervical and upper thoracic paravertebral
ganglia) nerves
TABLE 6 Diagnostic Criteria for the Most Common
DSM-IV Anxiety Disorders
|
DSM-IV CRITERIA FOR SIMPLE PHOBIA
Marked and persistent fear that is excessive
or unreasonable, cued by the presence or anticipation
of a specific object or situation (e.g., flying, heights,
animals, receiving an injection, seeing blood).
Exposure to the phobic stimulus almost invariably provokes
an immediate anxiety response, which may take the form
of a situationally bound or situationally predisposed
panic attack.
The person (adults only) recognizes that the feature is
excessive or unreasonable.
The phobic situation is avoided or is endured with intense
anxiety or distress.
The avoidance, anxious anticipation, or distress in the
feared situations interferes significantly with the person's
normal routine, occupational (or academic) functioning
or social activities or relationships or there is marked
distress about having the phobia.
DSM-IV DIAGNOSTIC CRITERIA FOR SOCIAL
PHOBIA
Marked fear of being focus of attention;
avoidance of meeting unfamiliar people and close scrutiny
by others
Fear of behaving in embarassing or humiliating way
Extreme anticipatory anxiety which may manifest as a panic
attack
DSM-IV DIAGNOSTIC CRITERIA FOR POSTrRAUMATIC
STRESS DISORDER
Experience of a traumatic event
Reexperienced by intrusive and distressing recollection,
dreams, flashbacks, distress in similar situations
Persistent avoidance of stimuli associated with trauma
Persistent symptoms of increased arousal
Duration of disturbance of at least 1 month
DSM-IV DIAGNOSTIC CRITERIA FOR PANIC
DISORDER
Recurrent and unexpected panic attacks
plus one or more of the following:
Persistent concern about having additional attacks (anticipatory
anxiety)
Worry about the consequences of the attacks
A significant change in behavior related to the attacks
(phobic avoidance) Not due to a substance, medical condition,
or mental illness
At least two unexpected panic attacks for diagnosis
DEFINITION OF PANIC ATTACK
A period of intense fear or discomfort
in which at least four of the following symptoms develop
suddenly
-Palpitations or increased heart rate -Chest pain or discomfort
-Sweating -Dizziness, light-headedness, or faintness
-Trembling or shaking -Derealization or depersonalization
-Sensations of shortness of breath or smothering -Fear
of losing control or going crazy
-Feeling of choking -Chills or hot flashes
-Nausea or abdominal distress -Paresthesia (numbness or
tingling)
-Fear of dying
DSM-IV CRITERIA FOR GENERALIZED ANXIETY
DISORDER
Excessive anxiety and worry for more
days than not for past 6 months
Difficulty controlling worry
Functional impairment and/or distress
Symptoms not attributable to other causes
Physical symptoms Psychological symptoms
Restlessness or feeling keyed up/on edge Excessive anxiety
or worry
Fatigue Difficulty controlling worry
Muscle tension Irritability
Difficulty concentrating or mind going blank
Sleep disturbance
|
Source: Reprinted with
permission from the Diagnostic and Statistical Manual of Mental
Disorders, 4th ed. Copyright 1994, American Psychiatric Association.