|
Causes of Cardiac Arrythmias
This
term refers to a change from a normal, regular, automatic, heart
beat and rhythm to an irregular beat and rhythm.
| 1.
Abnormalities of impulse generation |
A.
Change of normal automaticity
I. Normal sinus node pacemaker
(see figure 104b) failure in disease
states.
II. Normal sinus node excessively rapid due
to sympathetic nerve stimulation.
B. Pacemaker in His Bundle-Purjinke
system (see figure 104b) may control
cardiac rhythm as escape pacemakers or when sympathetic activity
is increased.
I.
Sinus bradycardia (see figure 16
and 17)
or AV block of atrial impulses to a rate lower than
intrinsic rate of His-Purjinke pacemaker.
II.
Abnormal conditions like ischemia (inadequate oxygen level
due to coronary atherosclerosis causing reduced blood flow)
or drug (medication) treatment increases rate of firing
of His-Purjinke system pacemaker to overcome the sinus node
rate.
C.
Abnormal automaticity in Purjinke cells ,which are
involved in a heart attack with ischemic fibers (reduced oxygen).
D.
Triggered activity is single or repetitive firing of a myocardial
cell or a group of cells caused by reexcitation (afterdepolarization
which occurs after repolarization has begun). Repolarization
is the electrochemical process of cell recovery after excitation
of the heart muscle.
I. There
are two kinds of afterdepolarization:
a.
early
Causes of early afterdepolarization
include:
1.
low potassium blood levels
2. slow heart rate (see figure 16)
3. drug toxicity (i.e. quinidine causing torsades
de pointes form of ventricular tachycardia, see figures
6,
13).
b. late (delated afterdepolarization
occur after the cell has repolarized).
These may cause rapid firing or triggered activity due to:
1. premature
beats
2. increased calcium blood levels
3. increased adrenaline levels
4. digitalis toxicity (see figure 4)
| 2.
Abnormalities of impulse conduction |
a. Slowing
of conduction and block (see figure 17)
b. Unindirectional block and reentry
(causes):
1.
Anomalous AV Connections that cause a short PR interval
and wide QRS (see figures
1, 3a).
This additional, anomalous pathway promotes rapid heart beats
called supraventricilar tachycardia. When this pathway is
destroyed, the tachycardia never reoccures (see figure
3b).
c.
Ordered reentry
d. Random reentry
| 3.
Combined abnormalities of impulse generation and conduction |
| 4.
NORMAL OR ABNORMAL IMPULSE INITIATION |
Automatic Rhythms Normal Mechanism
Cardiac cells that normally are capable
of developing spontaneous
diastolic (phase 4) depolarization are called pacemaker cells.
When pacemaker cells manifest spontaneous diastolic depolarization
(Fig. 16-1)
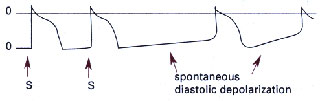
and thus are responsible for generating
the cardiac rhythm, the rhythm
is classffied as an automatic rhythm. Normally, the dominant
pacemaker
of the heart is in the sinus node, which in adults fires at
a rate of 60 to 100 beats per minute. Cells capable of developing
spontaneous diastolic depolarization (i.e., of manifesting automaticity)
also are normally found in the specialized fibers in the atria,
the atrioventricular (AV) junction, and the His-Purkinje system.
The normal rate of impulse formation in adults by these ectopic
pacemakers is 40 to 60 beats per minute in the AV junction (the
AV node and His bundle).
Normal rates of more distally located ectopic pacemakers are
probably
20 to 40 beats per minute in the bundle branches. These ectopic
(i.e.,
nonsinus) pacemakers also are called latent or escape pacemakers
for
two related reasons:
(1) The normal
intrinsic rate of these pacemakers is lower than that of the
dominant pacemaker, the sinus node, and
(2)
spontaneous diastolic depolarization of these latent or escape
pacemakers normally is suppressed by the more rapid rate of
the sinus node pacemaker through the active process of overdrive
suppression.
Only when the sinus rate slows below the intrinsic rate of these
ectopic pacemakers does "the next one in line" warm
up and fire (see also "Automaticity," below).
Arrhythmias of the Sinus Node
An arrhythmia occurs when the sinus
node pacemaker fires at a rate
above 100 beats per minute (sinus tachycardia) (Table 1) or
at a rate below
60 beats per minute (sinus bradycardia) and is still the dominant
pacemaker of the heart.
|
Tachycardia
|
Mechanism
|
Origin
|
Rate
Range, bpm
|
AV
or VA Conduction
|
| Sinus
tachycardia |
Automatic
(normal) |
Sinus
node |
>100
|
1:1
|
|
Sinus
nod reentry
|
Reentry
|
Sinus
node and right atrium
|
?110-180
|
1:1
or variable
|
|
Atrial
fibrillation
|
Reentry
|
Atria
|
260-450
|
Variable
|
| |
Fibrillatory
conduction
|
Pulmonary
veins, SVC
|
?
|
Variable
|
|
Atrial
flutter
|
Reentry
|
Right
atrium, left atrium (infrequent)
|
240-350,
usually 300 ± 20
|
2:1
or variable
|
|
Atrial
tachycardia
|
Reentry
|
Atria
|
150-240
|
1:1,
2:1, or variable
|
| |
Automatic
(normal or abnormal)
|
Atria
|
?
|
?
|
| |
Triggered
(DADs) 2° to digitalis toxicity
|
Atria
|
150-240
|
1:1,
2:1, or variable
|
| |
|
|
|
|
|
AV
nodal reentry tachycardia
|
Reentry
|
AV
node with an atrial component
|
120-250,
usually 150-220
|
1:1
|
|
AV
reentry (WPW or concealed accessory AV connection)
|
Reentry
|
Circuit
includes accessory AV connection, atria, AVnode, His,
Purkinje system, ventricles
|
140-250,
usually 150-220
|
1:1
|
|
Accelerated
AV junctional tachycardia
|
Automatic
or ? triggered (? digitalis toxicity)
|
AV
junction (AV node and
His bundle)
|
61-200,
usually 80-130
|
1:1
or variable
|
|
Accelerated
idioventricular rhythm
|
Abnormal
automaticity
|
Purkinje
fibers
|
>60-?
|
Variable,
1:1, or AV dissociation
|
|
Ventricular
tachycardia
|
Reentry
|
Ventricles
|
120-300,
usually 140-240
|
AV
dissociation, variable, or dissociation
|
| |
Automatic
(rare) (normal or abnormal)
|
Ventricles
|
?
|
Variable,
1:1, or AV dissociation
|
|
Bundle
branch reentrant
tachycardia
|
Reentry
|
Bundle
branches and ventricular septum
|
160-250,
usually 195-240
|
AV
dissociation, variable, or 1:1
|
|
Right
ventricular outflow tract
|
?
Triggered (DADs)
|
Right
ventricular outflow
tract
|
120-220
|
AV
dissociation, variable, or 1:1
|
|
Torsades
de pointes tachycardia
|
?
Triggered (EADs) (with reentry)
|
Ventricles
|
>200
|
AV
dissociation
|
Table 1
These are called arrhythmias resulting
from normal
automaticity, since the ionic mechanism causing the pacemaker
depolarization is unchanged from the normal sinus rhythm. A
sinus tachycardia is usually an appropriate response to a precipitating
factor (e.g., exercise, fever, hypotension), although on occasion
it may be inappropriate, as in the presence of a sympathetic
dysautonomia (inappropriate sinus tachycardia). By contrast,
sinus bradycardia often reflects an abnormality not only of
the sinus node pacemakers (they are too slow) but also of the
latent pacemakers (when the sinus rate slows abnormally, they
do not escape). Sinus bradycardia may be due to an intrinsic
abnormality of pacemaker cells, a parasympathetic dysautonomia
(inappropriate sinus bradycardia), or an extrinsic factor such
as suppression of automaticity by drug therapy (e.g., a beta
blocker, a Ca2~ channel blocker, or an antiarrhythmic agent).
Fro some patients, sinus bradycardia, particularly when it is
present only at rest, may simply reflect a normal response to
increased vagal tone, as in a well-trained athlete. Marked beat-to-beat
variations in cycle length of the sinus rhythm, which are due
virtually always to the influence of vagal tone on the pacemaker
cells of the sinus node, also is considered an arrhythmia (sinus
arrhythmia) even if the overall sinus rate is normal.
|