AV conduction may be delayed in either the AV node or the bundle of His. Delays in conduction below the bifurcation of Bundle of His cause bundle branch or fascicular blocks, while atrioventricular conduction is maintained, unless all three fascicles are simultaneously affected. The causes are both intrinsic and extrinsic. However, since the AV node and bundle of His provide a special connection of the atria to the ventricles, focal injury from heart attacks, infections, catheter trauma, is common.
 |
Mangrum, J.M., Dimarco, J.P., The Evaluation and Management of Bradycardia, NEJM 2000; 342, No. 10, 703-709 |
There are five different divisions of atrioventricular disturbances
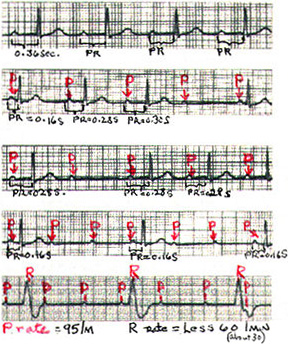
1) First-degree AV block is a common EKG finding. Values for the PR interval (the conduction time from the sinus node through the atrium, AV node, and His system to onset of ventricular excitation [depolarization]) over 0.2 second with a retained 1:1 AV relation is defined as first AV block (see top EKG of illustration). It does not cause Bradycardia itself, but in combination with higher degrees of AV block or sinus node dysfunction, can lead to bradycardia and symptoms, resolved by the use of a pacemaker (see figures 84-92).
Second-degree AV block occurs when an organized atrial rhythm fails to conduct to the ventricle in a 1:1 ratio, but some atrial-ventricular relation is maintained. Several varieties occur (see illustration, lower 4 EKG's).
2)
3) In second-degree AV block (called Mobitz type II) a stable P-P interval is present with no prolongation of the PR interval before an abrupt conduction failure (see EKG illustration, third from top).
This type block occurs with disease in the His-Purkinje system.
In AV block with 2:1 conduction ratio or higher (like 3:1 or 4:1) prolongation of the PR interval before the block is impossible to observe (so type I or II is not appropriate).
4) In 2:1 block, a narrow QRS complex (normal time of inscription) and associated periods of Wenchebach block, or simultaneous sinus slowing (vagus block), suggest that AV nodal block is present.
But a wide QRS complex (abnormally 1ong time of inscription) suggests the presence of infranodal block (i.e., His bundle).
5) In third degree AV block (complete block ) the atrial activity and ventricular activity are independent of each other (illustration, lower EKG).
Narrow QRS complexes (rates 40-60 beats per minute) suggest AV nodal block. Wide QRS escape rhythms at slower rates imply that the block is in the His-Purkinje system.
INDICATIONS FOR PERMANENT PACING
The indication for permanent pacemakers can be divided into three classifications (Table 1) and are listed in Table 2 according to the most recent indications published by a joint task force by the American College of Cardiology and the American Heart Associatioin in 1998.Many indications for pacemaker implanation are predicated by the presence of symptoms such as fatigue or subtle symptoms of congestive heart failure may be recognized only in retrospect, after placement of a permanet pacer maker.
Pacing in Acquired Atrrioventricular BLock
It is generally agreed that complete heart block,permanent or intermittent,at any anatomic level associated with symptoms such as dizziness ,lightheaded- ness ,syncope, congestive heart failure, or confusion is an indication for a permanent pacemaker.In the absence of symptoms,pacing is indicated for patients with third degree AV block,especially with awake heart rates of less than 40 beats per minute or pauses of longer than 3s.
In the presence of bifascicular or trifascicular block, intermittent third-degree or type 11 second-degree AV block usually indicates the need for a permanent pacemaker.When patients with these conduction patterns present with syncope,a pacemaker is usually required.However, an electrophysiologgy study may be useful to rule out other causes of syncope (e.g. ventricular tachycardia) particularly if structural heart disease is present.Additionally during electrophysiology study,permanent pacing may be indicated if there is markedly prolonged HV interval(>100ms.) or nonphysiologic pacing or drugs induced infraHis block.
Second-degree AV block associated with symptomatic bradycardia is an indication for pacing.In asymptomatic patients with second-degree AV block,type 11, cardiac pacing may be required if the level of the block is infranodal level.There are patients with bundle branch block or intraventricular block or intraventricular conduction delays in whom type 1 second-degree AV block is located at an infra nodal level.